This article as been adapted from this Berkeley Lab press release.
A technology developed by Foundry users shows great promise for diagnosing Alzheimer’s disease before symptoms arise, potentially changing the course of research and treatment for this condition, which affects millions of people worldwide and is estimated to be the sixth leading cause of death in the United States.
“This is a big deal,” said project leader Cynthia McMurray, following the publication of the team’s successful proof-of-principle study in the journal Scientific Reports. “Diagnosing Alzheimer’s disease at early stages is difficult and there is no way to predict who will get the disease, which means there is no successful pathway to develop therapeutics. However, this new technology uses accessible skin cells as surrogates to predict the disease status in the brain. We’re very excited for the possibilities of early prediction, before signs of disease have manifested.”
Alzheimer’s disease is the most common cause of dementia, yet despite decades of intensive research, the condition remains poorly understood. It can be definitively diagnosed only after death, with a brain tissue biopsy, and no existing medications can stop its progression.
The first step toward better research, new treatments, and improved quality of life for patients is a reliable diagnostic test. But how can we detect a disease when we don’t know what causes it in the first place?
Say hello to spectral phenotyping.
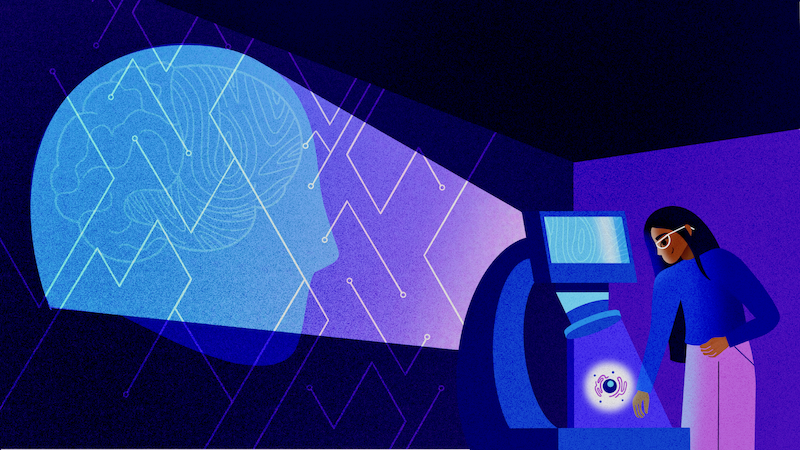
The new application of this technique developed by McMurray’s team analyzes cells for signs of disease by measuring how the molecules in cells vibrate upon exposure to infrared light. The vibrational profile of each sample is so distinct and the difference between diseased and healthy cell samples is so visible that McMurray likens the process to “cellular fingerprinting.”
“The actual physical phenomenon that we’re measuring with infrared light is the vibrational states of molecules in the cell,” said McMurray, who is a senior scientist in Berkeley Lab’s Biosciences Area.
All cells contain the same types of molecules, she explained, but infrared (IR) spectroscopy – a low-cost chemical analysis approach that has been around since the 1940s – can pick up extremely subtle differences in bonding and abundance of each molecule in a cell sample, including any abnormal changes that have occurred due to disease. “Even among cell types that look identical by other measures,” added McMurray.
Interested in Becoming a Foundry User?
Join our collaborative, multidisciplinary environment.
Learn more >
The subtle changes captured by the IR analysis, which produces datasets called spectra, are then detected by machine learning algorithms (a type of artificial intelligence known to excel at pattern recognition) that have been trained to differentiate between spectra of cells from individuals with disease and those without. This two-part testing platform allows the team to detect when something has gone wrong inside cells without needing to know what went wrong.
In their study, McMurray and colleagues confirmed the diagnostic potential of their approach by showing that an algorithm, developed in collaboration with Foundry staff member Ed Barnard, can easily distinguish IR spectra from mouse brain cells with Huntington’s disease from spectra of healthy mouse brain cells. Then, they trained an algorithm to do the same with human cells. It worked seamlessly.
Read the full press release.

